Detecting tumor cells during surgery

In cooperation with a hospital, Fraunhofer researchers have developed a technology that can determine far more quickly than previously whether a tumor has been completely removed, even while the patient is still in surgery. To achieve this, the consortium combined a compact laser scanning (LSC) microscope with fluorescent antibody-based tumor markers. This provides a way of telling immediately whether any cancer cells remain after the initial removal of the tumor. The detection process involves staining tissue outside the body with an antibody-based tumor marker and then examining it immediately at the critical tumor boundary using the LSC microscope.
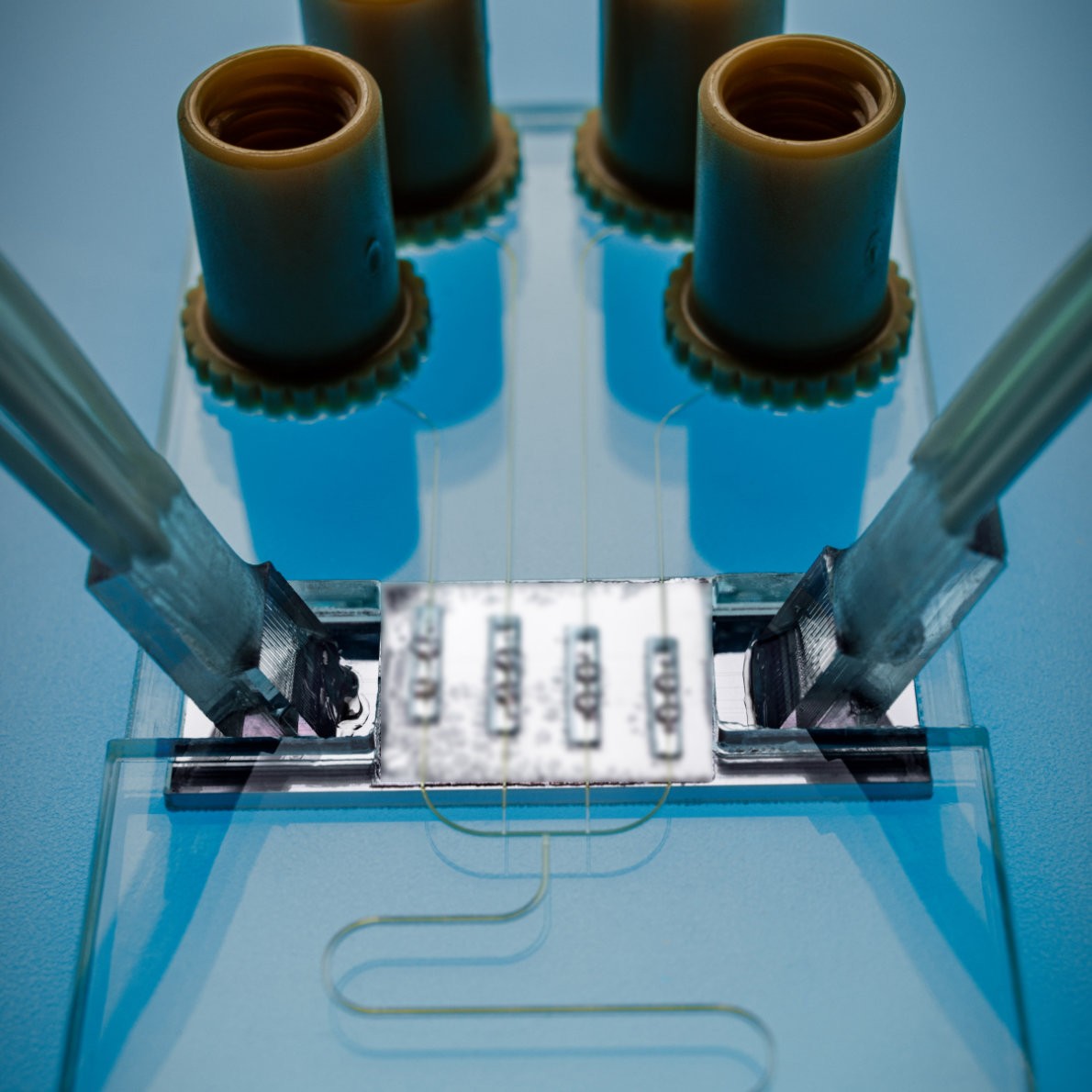
From a technological point of view, a 2D microscanning mirror produced with MEMS (Micro-Electronic-Mechanical Systems) is used for this purpose. It oscillates several thousand times per second within the microscope, directing blue and red laser light simultaneously and point by point over the entire image field with a lateral resolution of one micrometer. The mirror simultaneously directs the fluorescent light emitted by the tissue towards highly sensitive photodetectors. The signals from the photodetectors can then be used to construct a two-dimensional image. The resolution and precision of the system is so high that even individual cancer cells can be detected and shown on the display. Thanks to a confocal principle, images can also be captured on different planes. While the device development was ongoing, an antibody-based, tumor-specific staining method was tested to enable fluorescence imaging for both brain and skin tumors. Put simply, this makes the cancer cells glow under the microscope. The consortium is continuing to test the system in the hospital setting. In future, the system is expected to be combinable with imaging supported by artificial intelligence and robotic implementation.
For the first time, a powerful yet portable LSC microscope has been developed as part of the LSC-Onco (Laser Scanning Oncology) project. The LSC microscope can be placed in the operating room right next to the person being treated. The technology was jointly developed by Helios Klinikum Erfurt and the Fraunhofer Center for Microelectronic and Optical Systems for Biomedicine MEOS.